Laparoscopic roux-en y Gastric Bypass Bangladesh
- Home
- Laparoscopic roux-en y Gastric Bypass Bangladesh
Laparoscopic roux-en y Gastric Bypass Bangladesh
What is Laparoscopic Roux-en y gastric bypass?
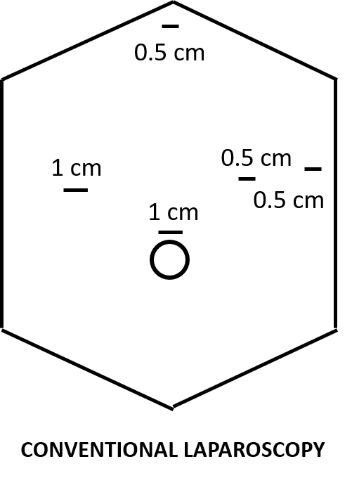
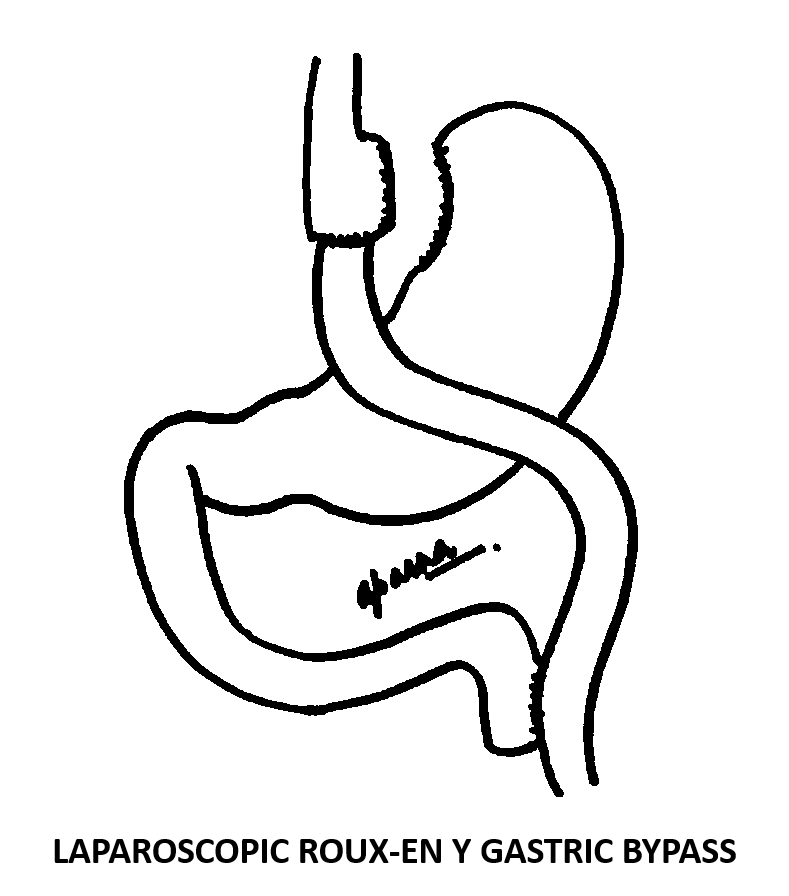
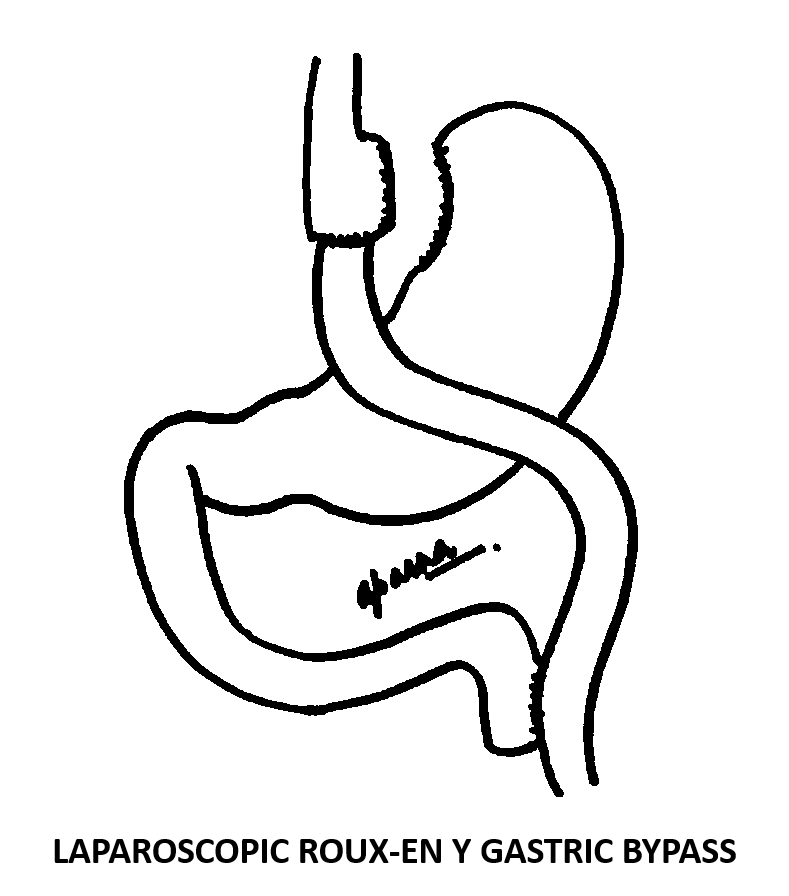
Laparoscopic Roux-en y gastric bypass is a surgical operation in which a small longitudinal pouch of the stomach is created using surgical staplers and the small intestine is rerouted and attached to the stomach in a Y shaped fashion. This procedure is performed laparoscopically through 5 tiny cuts on the abdomen as shown in the figure. In selected cases, an inflexible silicon band may be applied on the stomach pouch. This is called as banded Roux-en y gastric bypass. Band may prevent pouch dilatation and help in preventing weight regain in the long term.
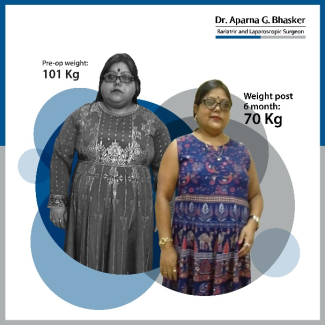
Patient review- Rupa Sen Chaudhary speaks about her weight loss journey after a laparoscopic Roux-en y gastric bypass –
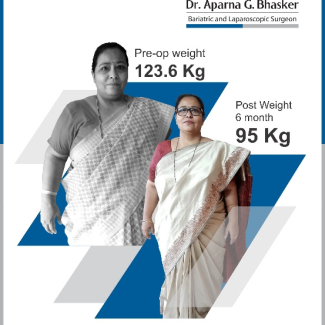
Patient review- Mr. Pradeep Seth-
What is the mechanism of action for weight loss after Laparoscopic Roux-en y gastric bypass?
As mentioned above, a laparoscopic Roux-en y gastric bypass entails creating a small stomach pouch alongwith re-routing of intestines. This leads to decreased oral intake and early satiety. The bypassed portion of the stomach contains the hunger hormone “ghrelin” which does not get activated and thus leads to a decrease in hunger. Gastric bypass surgery also leads to mal-absorption of calories and certain nutrients which adds to the weight loss. Other mechanisms like alteration in gut flora, bile acid interactions and neuro-hormonal changes have also been implicated for weight loss after gastric bypass surgery. It is important to note that weight-loss is a result of a combination of all the factors mentioned above and not just because of restriction of food intake alone.
In this video- Dr. Aparna Govil Bhasker speaks about laparoscopic Roux-en y gastric bypass-
What are the advantages of a Laparoscopic Roux-en y gastric bypass?
Laparoscopic Roux-en y gastric bypass is considered as one of the best bariatric operations and was called as the Gold-standard procedure across the world. It leads to better weight loss as compared to a sleeve gastrectomy. It has also shown better results in improvement of type 2 diabetes as compared to sleeve gastrectomy and other restrictive procedures. Laparoscopic Roux en y gastric bypass is the procedure of choice in patients suffering from gastro-esophageal reflux disease and hiatus hernia.
Who is a candidate for Laparoscopic Roux-en y gastric bypass?
The guidelines of the Obesity and Metabolic Surgery Society of India (OSSI) for patient selection are as under:
- Bariatric/metabolic surgery should be considered as a treatment option for acceptable Indian patients with a BMI ≥ 35 Kg/m2, with/without presence of any obesity related co-morbidity.
- Bariatric/metabolic surgery should be considered as a treatment option for acceptable Indian patients with a BMI ≥ 30 Kg/m2, in presence of two or more obesity related co-morbidities.
- Bariatric/metabolic surgery should be considered as a non-primary treatment option for acceptable Indian patients with a BMI ≥ 27.5 Kg/m2, with uncontrolled type 2 diabetes despite optimum medical management.
- Any bariatric/metabolic surgery for an Indian patient with BMI < 27.5 Kg/m2 should be strictly performed under experimental study protocol with prior ethics committee approval and informed consent from the patient.
- Bariatric/metabolic surgery should be considered as a treatment option for acceptable Indian patients with central obesity with a waist circumference ≥ 80 cm in females and ≥ 90 cm in males along with type two diabetes and other obesity related co-morbidities.
- Bariatric/metabolic surgery may be advised as a treatment option for acceptable Indian patients who qualify for the above BMI criteria if they are ≥ 18 years of age. It may be advised as a treatment option to patients younger than 18 years of age under special circumstances with approval of a multi-disciplinary team constituting a paediatrician, endocrinologist, dietician, psychologist and the bariatric team including a bariatric surgeon. Attainment of puberty and completion of skeletal maturity must be taken into account for this patient population when considering the option of surgery.
- Bariatric/metabolic surgery should be advised as a treatment option for acceptable Indian patients who qualify for the above BMI criteria for patients up to 65 years of age. Bariatric/metabolic surgery may also be recommended for patients ≥ 65 years of age if they are medically fit and the benefits of surgery outweigh the risks.
- All patients who are advised bariatric/metabolic surgery as a treatment option should be motivated to enter a long-term weight management program and should be committed to life-long follow up.
- Long term weight management program and follow up must be provided by all bariatric teams
Who should not undergo Laparoscopic Roux-en y gastric bypass?
As per the guidelines of the Obesity and Metabolic Surgery Society of India (OSSI) for patient selection the contra-indications for Laparoscopic Roux-en y gastric bypass are as under:
- Bariatric/metabolic surgery may not be advised as a treatment option to a patient who is unable to adhere to prolonged follow up program or express inability to take nutritional supplements.
- Bariatric/metabolic surgery may not be advised as a treatment option to patients who are medically unfit to undergo a surgery.
- Bariatric/metabolic surgery may not be advised as a treatment option to patients with non-stabilized psychiatric disorders.
- Bariatric/metabolic surgery may not be advised as a treatment option to chronic smokers, chronic alcoholics or patients with drug dependencies unless they have been through a deaddiction program successfully.
- Bariatric/metabolic surgery may not be advised as a treatment option to patients who have a short life expectancy or are suffering from a terminal illness.
- Bariatric/metabolic surgery may not be advised as a treatment option to pregnant women or those who wish to conceive within one year after surgery.
What is the pre-surgery preparation before Laparoscopic Roux-en y gastric bypass?
After consultation with our bariatric surgeon and the team, you will be advised to get investigations done. Once the reports come in, you will be seen by other specialists like the endocrinologist, hepatologist, chest physician, psychologist, nephrologist etc depending on your clinical profile. You will also be seen by the anaesthesia team for requisite fitness.
Along with this, you will be advised to start on a 7 days pre-surgery high protein liquid diet. Our team of dieticians will guide you through this phase. In case your tests reveal any abnormalities or nutritional deficiencies, correction is advised prior to the surgery.
Video of UGI endoscopy-
How is the recovery after Laparoscopic Roux-en y gastric bypass?
Laparoscopic Roux-en y gastric bypass is performed under general anaesthesia. Patient is awake soon after the surgery gets over. We encourage our patients to mobilize out of the bed and walk for a short distance within 4 to 6 hours after surgery. Generally, no urinary catheters are inserted. This motivates the patients to get up and walk to the washroom. Oral liquids are started from the next day and continued for 15 days. After this soft diet is advised for another 15 days. Patients can start normal diet after one month from surgery, however, this is highly restricted in quantity.
Most of the aches and pains at the incision sites settle down within a week of surgery and patients generally are able to get back to work after seven to ten days. Mild activity is encouraged even in the first week of surgery.
What is the diet protocol after Laparoscopic Roux-en y gastric bypass?
Day of surgery- Nil by mouth (fasting)
Day 1 & Day 2- Clear liquid diet
Day 3 to day 15- Full liquid diet
Day 15 to day 30- Soft/pureed diet
Day 31 onwards- Normal diet (Restricted in quantity)
How much time does it take to lose weight after Laparoscopic Roux-en y gastric bypass?
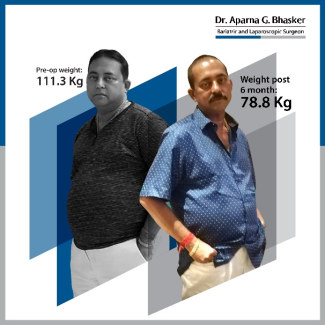
Weight loss is gradual after any bariatric operation and it normally takes about 12 to 18 months to reach the nadir weight. In the first 3 to 6 months patients lose weight quite fast and lose upto 50% of their excess weight. After that it tends to slow down but they continue to lose weight till about 18 months.
Does Laparoscopic Roux-en y gastric bypass lead to any improvement in other associated diseases of obesity?
All bariatric operations including Laparoscopic Roux-en y gastric bypass lead to improvement in diseases associated with obesity. The average improvement in associated diseases is listed in the table below:
SN |
OBESITY ASSOCIATED DISEASES |
EFFECT OF BARIATRIC SURGERY |
PERCENTAGE IMPROVEMENT |
1 |
Quality of life |
Improves |
Upto 95% |
2 |
Relative risk of mortality |
Decreases |
Upto 89% in 5 years |
3 |
Metabolic Syndrome |
Improves |
Upto 80% |
4 |
Type 2 diabetes |
Improves |
82 -98% |
5 |
High blood pressure |
Improves |
60 -70% |
6 |
Hypercholesterolemia |
Improves |
60-65% |
7 |
Risk of heart disease |
Decreases |
|
8 |
Obstructive sleep apnoea |
Improves |
74 – 98% |
9 |
PCOD |
Improves |
Upto 75% |
10 |
Venous stasis disease |
Improves |
Upto 95% |
11 |
Osteo-arthritis/Joint disease |
Improves |
Upto 41% |
12 |
Urinary stress incontinence |
Improves |
Upto 44% |
13 |
Depression |
Improves |
Upto 47% |
14 |
Gout |
Improves |
Upto 72% |
15 | Infertility |
Improves |
What are the side effects of Laparoscopic Roux-en y gastric bypass?
The complication rate after Laparoscopic Roux-en y gastric bypass is less than 2%. Staple line leaks, venous thrombo-embolism and haemorrhage are some of the early complications. Strictures, marginal ulcers, internal herniation and weight regain are some of the issues that are seen in some patients in the long term. The doctor and the team will discuss and explain these to you in detail during your consultation.
Is Laparoscopic Roux-en y gastric bypass a safe operation?
Yes, Laparoscopic Roux-en y gastric bypass is a safe operation. Complication rate after Laparoscopic Roux-en y gastric bypass is similar to that of a gall bladder surgery or a knee replacement surgery. Infact, it is considered to be safer than other major operations like a cardiac bypass surgery or surgery for oesophageal cancer etc. However, all bariatric operations must be carried out at a good centre by an experienced surgeon. It is important that the centre has a multi-disciplinary team to look after the patient.
What is the impact on pregnancy?
Many female patients who suffer from obesity also have associated PCOD. Many a times they find it difficult to conceive even with the help of assisted reproduction techniques like IUI and IVF. Weight loss induced by any kind of bariatric surgery helps to improve PCOD and also improves fertility. However, it is advisable to avoid pregnancy in the first year after any bariatric surgery as this is the active weight loss period and the oral intake is lower in the first few months after surgery. Many women conceive after that and have normal pregnancies. It is also advisable to consult the bariatric team and have a complete nutritional evaluation before planning a pregnancy.
Will I need to take nutritional supplements after Laparoscopic Roux-en y gastric bypass?
Yes, nutritional supplements are required after any weight loss surgery and especially after Laparoscopic Roux-en y gastric bypass. After a gastric bypass, the stomach and first part of small intestine is bypassed and hence the absorption of certain nutrients like vitamins, calcium and iron is hampered. Hence it is important to take these supplements for life.
Is it necessary to take protein supplement after Laparoscopic Roux-en y gastric bypass?
Protein supplementation is necessary after all bariatric surgeries. A normal person’s protein requirement is 1 gm/kg of their ideal body weight. That means that most of us need a minimum of 45 to 60 grams of protein per day. After Laparoscopic Roux-en y gastric bypass, oral intake decreases and protein absorption is also hampered, hence it is important to fulfil the daily requirement of protein, using supplements. Protein intake helps us to maintain and preserve the muscle mass.
What is the follow up protocol after Laparoscopic Roux-en y gastric bypass?
After Laparoscopic Roux-en y gastric bypass patients are advised to visit the doctor and the bariatric team at following intervals:
- 7 days
- 1 month
- 3 months
- 6 months
- 12 months
- 18 months
- 24 months
- Once every year from the third year onwards.
Every follow up visit entails doing investigations as advised by the team and coming in for a face to face consultation. If you stay far away and it is not possible for you to come, then an online consultation can be done and you can send your reports to us on email for evaluation. Follow up is a joint responsibility. The follow up schedule will be provided to you after your surgery and we will also send regular reminders to you. However, it is a two-way street and we expect our patients to also get in touch with us whenever the follow up is due. In this video Miloni Sancheti talks about the importance of follow up after bariatric surgery-
In this video, Miloni Sancheti speaks about activity after bariatric surgery-
Can one regain weight after Laparoscopic Roux-en y gastric bypass?
Obesity is a chronic progressive disease. Bariatric surgery is a tool that helps to reduce massive amount of weight and is currently the only effective method for weight loss in people suffering from severe obesity. However, to maintain this weight loss, a fair amount of work is required from the patient. Lifestyle modification, exercise and a healthy diet go a long way in maintain weight loss. Patients who embrace lifestyle modification, maintain their weight much better than those who do not. Weight regain can happen after any bariatric procedure, but patients who embrace lifestyle modification tend to maintain their weight much better.
What is the cost of Laparoscopic Roux-en y gastric bypass?
The cost of Laparoscopic Roux-en y gastric bypass varies as per the room type chosen and the hospital in which the surgery is performed. We offer quality care for affordable cost so that more people can avail good treatment. Specific details about the cost will be provided to you at the time of consultation with the team.
Is Laparoscopic Roux-en y gastric bypass covered by health insurance in India?
In a recent development in October 2019, the Insurance and Regulatory Authority of India has included bariatric surgery under insurance coverage. However, it will take some more time to get clarity on the qualifying criteria, the waiting time etc. We always encourage our patients to apply to their insurance companies.
About Dr. Aparna Govil Bhasker
Dr. Aparna Govil Bhasker is an accomplished Bariatric Surgeon and Laparoscopic GI Surgeon. Extremely passionate about her field of specialization. She completed her MBBS and MS in General Surgery in 2006, from Mahatma Gandhi Institute of Medical Sciences (MGIMS), Sewagram. Set up in 1967 by none other than the first health minister of India, Ms. Sushila Nayar, MGIMS is deeply rooted in Gandhian ethics. Read more
Surgeon in India


Bariatric Surgery: Pros and Cons
Types of Hernias and Their Treatment Options Explained
- Intra-Gastric Balloon Insertion Surgery
- Laparoscopic Adjustable Gastric Banding Surgery
- Gastric Sleeve Surgery / Laparoscopic Sleeve Gastrectomy
- Single Incision Sleeve Gastrectomy Surgery
- Laparoscopic Roux-en Y Gastric Bypass Surgery
- Laparoscopic Banded Roux-en Y Gastric Bypass Surgery
- Laparoscopic Mini Gastric Bypass Surgery /Omega Loop Bypass
- Laparoscopic Sleeve Gastrectomy with Duodeno-Jejunostomy Surgery
- Laparoscopic Duodenal Switch Surgery
- Laparoscopic Sleeve Gastrectomy with Duodenal Ileostomy (SADI) Surgery
- Laparoscopic Revisional/Redo Bariatric Surgery
- Metabolic Surgery for Diabetes
- Terms & Conditions
- Privacy Policy
- Sitemap